Atypical Trigeminal Neuralgia (Atypical TN) and Atypical Facial Pain
If you’re living with constant facial pain, burning, aching, or pressure—especially when it doesn’t fit the “classic” trigeminal neuralgia pattern—you may have heard terms like atypical trigeminal neuralgia, atypical TN, TN2, or even atypical facial pain.
These labels can be confusing. The good news is this: you are not alone, and there are real treatment options. The first step is an accurate diagnosis and a clear plan.
Dr. Ramesh P. Babu, M.D. evaluates complex facial pain conditions, including atypical trigeminal neuralgia and facial pain that may be linked to nerve compression, multiple sclerosis, or skull base tumors. If you’re looking for an experienced NYC neurosurgeon to help you understand your facial pain and your options, we’re here to help.
What Is Atypical Trigeminal Neuralgia?
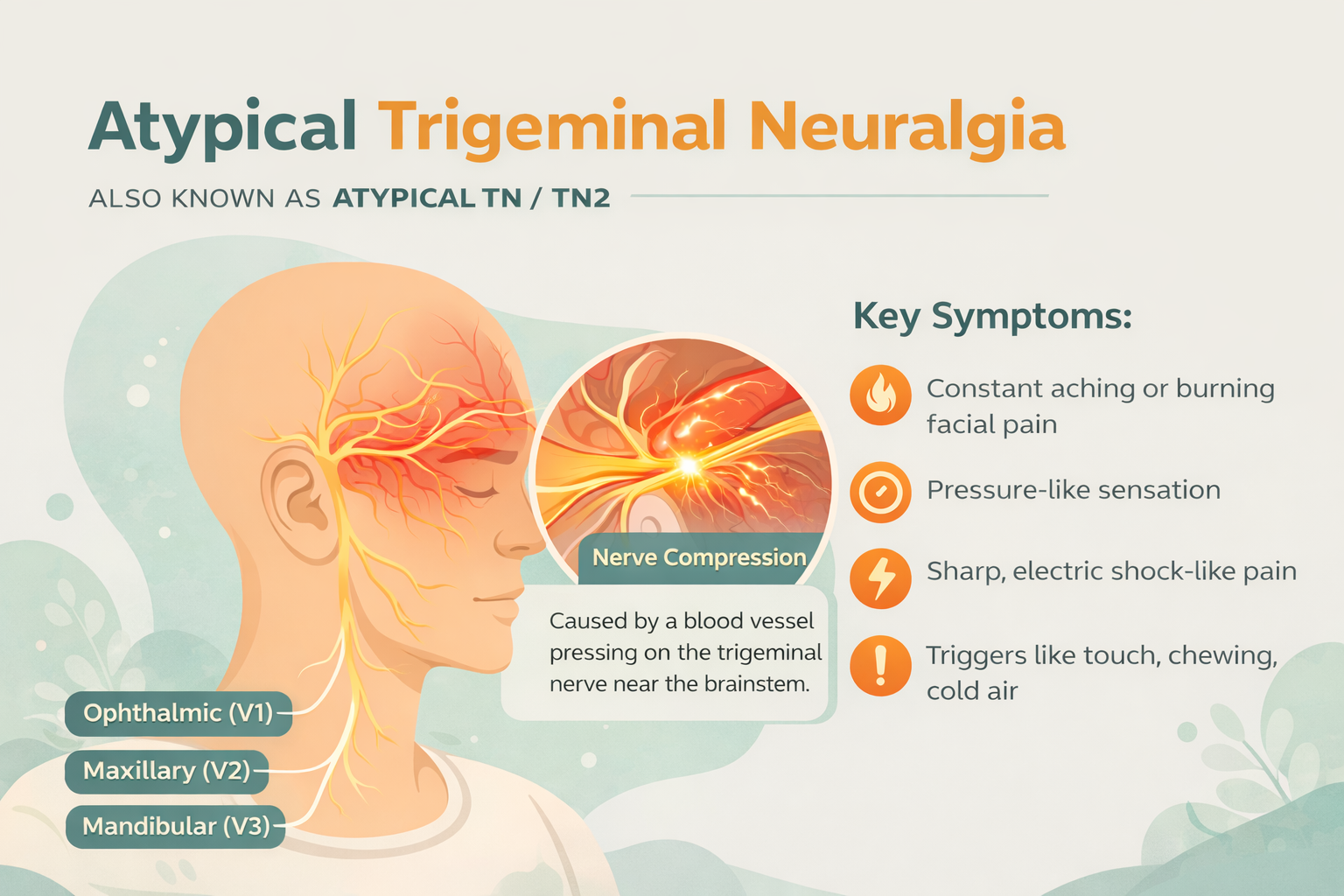
Atypical trigeminal neuralgia (atypical TN) is often used to describe trigeminal neuralgia that includes:
A constant or near-constant background pain (aching, burning, pressure), plus
Sudden flares that can feel sharp, stabbing, or electric
Many specialists call this Trigeminal Neuralgia Type 2 (TN2). Some medical classifications describe it as trigeminal neuralgia “with continuous pain between attacks.”
How Is Atypical TN Different From “Classic” Trigeminal Neuralgia?
Classic trigeminal neuralgia (sometimes called TN1) is best known for:
Sudden, brief, shock-like attacks
Clear triggers (like chewing, brushing teeth, touching the face)
Little or no pain between attacks
Atypical TN (TN2) may include:
More constant pain, sometimes daily
Pain that can be burning, aching, or heavy
Flares that still may be triggered by touch, eating, talking, or cold air
A pattern that can overlap with other facial pain conditions
Because the symptoms can overlap, a careful evaluation matters.
Atypical Facial Pain vs. Atypical Trigeminal Neuralgia
You may also hear the term “atypical facial pain.” Some doctors use it loosely to mean “facial pain that doesn’t fit the usual pattern.” But in many medical settings, “atypical facial pain” refers to a separate condition often called persistent idiopathic facial pain.
In simple terms:
Atypical TN / TN2 often still follows the trigeminal nerve “map” and may include sharp flares.
Atypical facial pain may feel more widespread, dull, or hard to pinpoint—and may not have classic triggers.
These conditions can feel similar, but the best treatments can be very different. That’s why it’s important to see a specialist who treats facial pain regularly.
Common Symptoms of Atypical TN
People describe atypical trigeminal neuralgia in many ways. Common symptoms include:
Constant aching or burning pain on one side of the face
Pressure-like facial pain
Sharp “flare” attacks on top of the constant pain
Pain in the:
Cheek, upper jaw, teeth area
Lower jaw
Nose or around the eye
Forehead (less common)
Pain triggered or worsened by:
Chewing or talking
Brushing teeth
Shaving or putting on makeup
Light touch
Wind, cold air, or air conditioning
Some people also notice:
Sleep disruption
Anxiety about the next flare
Avoiding eating, speaking, or social activities
This is real pain, and it deserves real care.
What Causes Atypical Trigeminal Neuralgia?
Atypical TN can happen when the trigeminal nerve is irritated. Possible causes include:
A blood vessel pressing on the trigeminal nerve (called neurovascular compression)
Multiple sclerosis (MS) (in some patients)
A tumor or growth near the trigeminal nerve (less common, but important to rule out)
Prior injury or irritation to the nerve (in some cases)
Sometimes, imaging does not show a clear cause. Even then, treatment may still help—especially when symptoms match trigeminal nerve pain.
How Atypical Trigeminal Neuralgia Is Diagnosed
There is no single “one-step” test. Diagnosis usually includes:
1) A Detailed Pain History
We’ll talk about:
Where the pain is
What it feels like (burning, aching, shocks)
Triggers
How long it lasts
What medications or dental work you’ve tried
2) A Focused Neurologic Exam
This checks facial sensation and other nerve functions.
3) Imaging (Often an MRI)
An MRI helps look for:
Nerve compression by a blood vessel
MS-related changes
Tumors or other structural causes (including skull base tumors)
4) Sorting Out “Look-Alike” Conditions
Some conditions can mimic atypical TN, including:
Dental problems (tooth, gum, bite issues)
TMJ disorders
Migraine or cluster headache
Sinus disease
Post-herpetic pain (after shingles)
Other nerve pain conditions
Getting the diagnosis right is key—especially before considering a procedure.
Treatment Options for Atypical TN (TN2)
Treatment depends on your exact pain pattern, imaging, medical history, and how the pain is affecting your life.
Medications (Often the First Step)
Many patients start with nerve-stabilizing medicines, such as:
Anti-seizure nerve pain medications (commonly used for TN)
Other neuropathic pain medications
Sometimes muscle relaxants or other supportive medicines
Medication goals:
Fewer flares
Less background pain
Better daily function
Important: These medicines can have side effects and may require monitoring. Your care team will discuss what to watch for and coordinate with your other doctors as needed.
Nonsurgical Options
Depending on your situation, options may include:
Targeted nerve blocks (diagnostic and/or short-term relief)
Other pain-management strategies guided by your diagnosis
Procedures and Surgery
If medications don’t work well—or side effects limit treatment—procedures may be considered.
Common options include:
Microvascular Decompression (MVD)
If imaging suggests a blood vessel is compressing the trigeminal nerve, MVD may be an option.
Goal: relieve pressure on the nerve without intentionally damaging it
Best results often happen when there are clear, shock-like attacks, but some patients with atypical TN also improve—especially when compression is seen.
Stereotactic Radiosurgery (Gamma Knife)
A focused radiation treatment aimed at the nerve.
No incision
Relief may be gradual
May be a good option for some patients who are not ideal surgical candidates.
Percutaneous Procedures (Minimally Invasive)
These procedures treat the nerve through a needle-based approach.
They can reduce pain but may cause facial numbness in some patients.
The “right” procedure depends on your pain pattern, your MRI, your health, and your goals.
Why Patients Seek a Specialist for Atypical TN
Atypical trigeminal neuralgia and atypical facial pain are often:
Misdiagnosed
Treated for the wrong problem (for example, repeated dental work that doesn’t help)
Dismissed because symptoms don’t sound “classic”
A specialist evaluation helps you answer:
“Is this really trigeminal neuralgia type 2?”
“Is there nerve compression?”
“Could this be related to MS or a skull base tumor?”
“What treatments fit my specific pattern of pain?”
What to Expect at a Consultation With Dr. Babu
During your visit, you can expect a careful, step-by-step approach:
Listening to your full story (including what hasn’t worked)
Reviewing imaging and prior treatments
Explaining the likely diagnosis in plain language
Discussing all reasonable options—medications, procedures, and surgery
Helping you weigh benefits and risks based on your goals
When Facial Pain Needs Urgent Medical Attention
Most facial pain is not an emergency—but seek urgent care if you have:
New facial numbness or weakness
New double vision, severe dizziness, or trouble speaking/swallowing
A sudden “worst headache” or new severe neurologic symptoms
Fever with facial swelling or severe dental infection symptoms
If you’re unsure, it’s always safer to get checked.
Dr. Ramesh P. Babu Q&A (Patient Questions)
People keep telling me “atypical TN.” What does that actually mean?
Dr. Babu: Many patients use “atypical trigeminal neuralgia” to describe TN with constant pain between attacks. You may still have flares that feel sharp or electric, but you also have a daily background ache or burn. The goal is to name the pattern correctly so we can choose the right treatment.
How do you tell atypical TN from atypical facial pain?
Dr. Babu: I start by mapping the pain and listening for key features—triggers, flare patterns, and whether the pain follows the trigeminal nerve distribution. I also look closely at imaging to rule out structural causes. These conditions can overlap, so careful evaluation matters.
Can atypical TN be caused by a blood vessel pressing on the nerve?
Dr. Babu: Yes. In many patients, the trigeminal nerve is irritated by neurovascular compression. When we see that clearly, it can guide decisions about options like microvascular decompression.
Do I need an MRI?
Dr. Babu: In most patients with suspected trigeminal neuralgia—especially when symptoms are atypical—an MRI is important. It helps us check for compression, MS-related changes, or rare causes like a tumor.
What is the first treatment you usually try?
Dr. Babu: We typically begin with medications designed for nerve pain, chosen based on your symptoms and medical history. The goal is meaningful pain control with acceptable side effects.
When do you consider surgery for atypical trigeminal neuralgia?
Dr. Babu: If pain remains severe despite good medication trials, or if side effects are limiting, we talk about procedures. The best option depends on your MRI findings, the type of pain you have, and your overall health.
Does surgery “cure” atypical TN?
Dr. Babu: Some patients do very well, especially when there is clear nerve compression and clear TN-type flares. With atypical TN, results can be more variable. My focus is to give you an honest, personalized picture of what improvement may look like—and which option best matches your goals.
What if I have multiple sclerosis (MS) or a skull base tumor?
Dr. Babu: Trigeminal neuralgia can sometimes be linked to MS or a structural cause. In those situations, the treatment plan may be different. This is where a detailed workup and specialist care can make a big difference.
I’ve had dental work that didn’t help. Does that rule out atypical TN?
Dr. Babu: Not at all. Facial nerve pain is often mistaken for dental pain. Part of my job is to help you sort out where the pain signal is truly coming from.
Is atypical trigeminal neuralgia the same as TN2?
Dr. Babu: Often, yes. Many people use atypical TN to mean trigeminal neuralgia type 2 (TN2)—pain with a more constant background ache or burn.
What does atypical TN pain feel like?
Dr. Babu: Many patients feel a constant aching, burning, or pressure-like pain, with flares that may be stabbing or shock-like.
Can atypical TN affect both sides of the face?
Dr. Babu: It’s most often one-sided. Bilateral symptoms can happen, but it’s less common and deserves careful evaluation.
Can it feel like tooth pain?
Dr. Babu: Yes. Atypical TN can feel like pain in the teeth or jaw. That’s why some patients go through dental procedures before getting the correct diagnosis.
What triggers atypical TN flares?
Dr. Babu: Common triggers include chewing, talking, brushing teeth, touching the face, shaving, and cold air or wind.
How long do flares last?
Dr. Babu: Flares can be brief (seconds to minutes) or come in waves. The background pain may last much longer.
Is atypical facial pain the same thing?
Dr. Babu: Not always. “Atypical facial pain” is sometimes used to describe facial pain that doesn’t match classic TN. But it can also refer to a different diagnosis. A specialist evaluation helps clarify this.
What medications are commonly used?
Dr. Babu: Doctors often start with medications that calm irritated nerves. The best choice depends on your symptoms and your health history.
What if medication helps, but I can’t tolerate side effects?
Dr. Babu: That’s a common problem. If side effects limit treatment, we can discuss other medication strategies or procedural options based on your diagnosis.
What procedures can help atypical TN?
Dr. Babu: Depending on the cause and your health, options may include microvascular decompression (MVD), Gamma Knife, or minimally invasive needle-based procedures.
How do I know if I’m a candidate for MVD?
Dr. Babu: MVD is most often considered when imaging suggests a blood vessel compressing the trigeminal nerve, and when symptoms fit a TN pattern. Your consultation and MRI review are key.
What should I bring to my appointment?
Bring:
A list of medications you’ve tried (and side effects)
Copies of MRI/CT images (if you have them)
Notes on triggers and pain patterns
Prior dental, ENT, or neurology records (if available)
What questions should I ask during my consult?
Good questions include:
“What diagnosis best matches my symptoms?”
“Do you see nerve compression on my MRI?”
“What are my treatment options and the pros/cons of each?”
“What results are realistic for my pain pattern?”
Ready to Get Answers?
If you think you may have atypical trigeminal neuralgia, TN2, or atypical facial pain, a focused specialist evaluation can help you move from uncertainty to a clear plan.
Request a consultation with Dr. Ramesh P. Babu, M.D. to review your symptoms, imaging, and treatment options.