Facial Pain: What’s Causing It? A Step-by-Step Guide to Getting the Right Diagnosis
Facial pain is one of those symptoms that can be simple (like sinus pressure) or surprisingly complex (like nerve pain). It can show up in your jaw, teeth, cheek, around your eye, or across one side of your face. It might be stabbing, throbbing, burning, or feel like electric shocks. And the right diagnosis depends less on “where it hurts” and more on the pattern. [1]
This step-by-step guide walks you through how facial pain is typically evaluated so you can get to the right specialist faster, avoid unnecessary detours, and get a plan that actually fits.
This blog is educational and not medical advice. If your symptoms are severe, new, or worsening, get medical care.
Step 0: Rule out red flags first
Most facial pain is not an emergency, but some combinations of symptoms should be treated as urgent. [1]
Call 911 or go to the ER if facial pain happens with:
Stroke symptoms (think FAST: Face drooping, Arm weakness, Speech difficulty, Time to call 911). [12]
Chest, arm, shoulder, or neck pain that could suggest a heart problem, especially with shortness of breath, sweating, or nausea. [1]
High fever and swelling around the eye, bulging eye, or worsening eye pain (this can be an emergency). [14]
Confusion, double vision, vision changes, stiff neck, or severe swelling around the eyes with sinus symptoms. [6]
New headache with scalp tenderness, jaw pain when chewing, and any vision symptoms (giant cell arteritis needs urgent evaluation to help prevent vision loss). [13]
If none of those apply, keep going.
Step 1: Name the pain pattern (this is the biggest clue)
Use this quick “pattern cheat sheet” to describe what you’re feeling.
Electric, shock-like, triggered by touch
If pain comes as sudden, intense “zaps” or stabbing shocks triggered by things like brushing teeth, chewing, talking, shaving, or even a light breeze, that pattern is often consistent with trigeminal neuralgia. [2][3]
Dull, aching, daily pain that doesn’t follow a nerve line
If pain is persistent, present daily, and feels poorly localized (often described as dull, aching, or nagging), one diagnosis doctors consider after other causes are ruled out is Persistent Idiopathic Facial Pain (PIFP), previously called atypical facial pain. [10]
Pressure or tenderness in cheeks/forehead, worse bending over
Facial pressure, tenderness, swelling around the face or eyes, nasal congestion, and pain that worsens when bending forward can point toward sinusitis. [6]
Jaw pain, chewing pain, clicking, or locking
Pain in the jaw joint or jaw muscles, trouble chewing, facial aching near the ear, clicking, or jaw locking can fit TMJ disorders. [5]
Severe pain around one eye with tearing or a runny/stuffy nose
Cluster headache pain is often severe, one-sided, and centered around or behind one eye, and can come with tearing, nasal symptoms, or eyelid changes on the painful side. [8]
Burning/tingling pain with (or after) a rash
Shingles can affect the face. Pain, tingling, or sensitivity may come before the rash appears. A key complication is postherpetic neuralgia (nerve pain that can persist long after the rash). [9]
Tooth-centered pain, swelling, or a “bad taste”
A dental infection like a tooth abscess can cause significant pain and swelling, and it needs treatment. Left untreated, infection can spread. [11]
Step 2: Map the pain location and side (without over-weighting it)
Facial pain can affect one side or both. People describe it as stabbing, dull, throbbing, tingling, or shooting. [1]
That said, location can still help narrow things down:
Around the eye/forehead (V1), cheek/upper jaw (V2), or lower jaw (V3) may suggest trigeminal nerve involvement, especially if the pain is shock-like or triggered. [3]
Jaw joint area (in front of the ear) often points more toward TMJ. [5]
Cheeks/forehead with congestion leans more sinus-related. [6]
Tooth-specific pain leans dental (but nerve pain can mimic tooth pain, so pattern matters). [2][11]
Step 3: Check for “bonus symptoms” that steer the diagnosis
These associated symptoms can change the whole direction of the workup:
Nasal congestion, postnasal drip, facial pressure, fever → more consistent with sinusitis. [6]
Light sensitivity, nausea, smell sensitivity, dizziness → common migraine-associated features. [7]
Tearing, runny nose, eye redness on one side during attacks → common in cluster headaches. [8]
Rash (or pain before rash), blistering on the face → consider shingles. [9]
Numbness, weakness, or new neurologic symptoms → needs prompt evaluation. [1]
Vision problems with temple headache or jaw pain when chewing → giant cell arteritis is a concern and should be treated urgently. [13]
Step 4: Keep a short symptom log for 7 days (it speeds up diagnosis)
Bring your doctor data, not just “it hurts.”
Track:
When attacks happen (time of day, frequency)
How long they last
Exact triggers (touch, chewing, wind, stress, sleep)
Where the pain starts and where it spreads
Any associated symptoms (tearing, congestion, nausea, rash, numbness)
What helps and what does nothing
This kind of tracking is often recommended in headache and migraine care, and it’s equally helpful for facial pain workups. [7]
Step 5: Know who to see first (and when to escalate)
A practical pathway most patients follow:
Start with your primary care clinician (or urgent care if severe)
They can screen for red flags, infection, neurologic changes, and guide you to the right specialty. Persistent or unexplained facial pain should be evaluated. [1]
See a dentist if pain feels tooth-based
Trigeminal neuralgia and other facial pain conditions can mimic dental pain, so a dental exam is often part of the process. [2]
If an abscess is suspected, dental imaging may be used, and severe infection requires prompt treatment. [11]
Consider ENT if symptoms are sinus-heavy
Sinusitis can cause facial pain, pressure, and swelling, and certain warning signs (eye swelling, high fever, confusion, vision changes) require urgent evaluation. [6]
Neurology vs neurosurgery
Neurology is often helpful when migraine, cluster headache, or broader neurologic issues are suspected. [7][8]
Neurosurgery is often involved when symptoms strongly suggest trigeminal neuralgia, when medications are not tolerated or stop working, or when imaging is needed to evaluate possible nerve compression or secondary causes. [4]
Step 6: Understand what “diagnosis” usually includes
Most facial pain diagnoses come down to a careful history + exam. After that, testing is targeted.
Common pieces of the workup may include:
Focused neurologic exam (especially for suspected nerve pain). [4]
Dental evaluation and X-rays if infection or tooth pathology is suspected. [11]
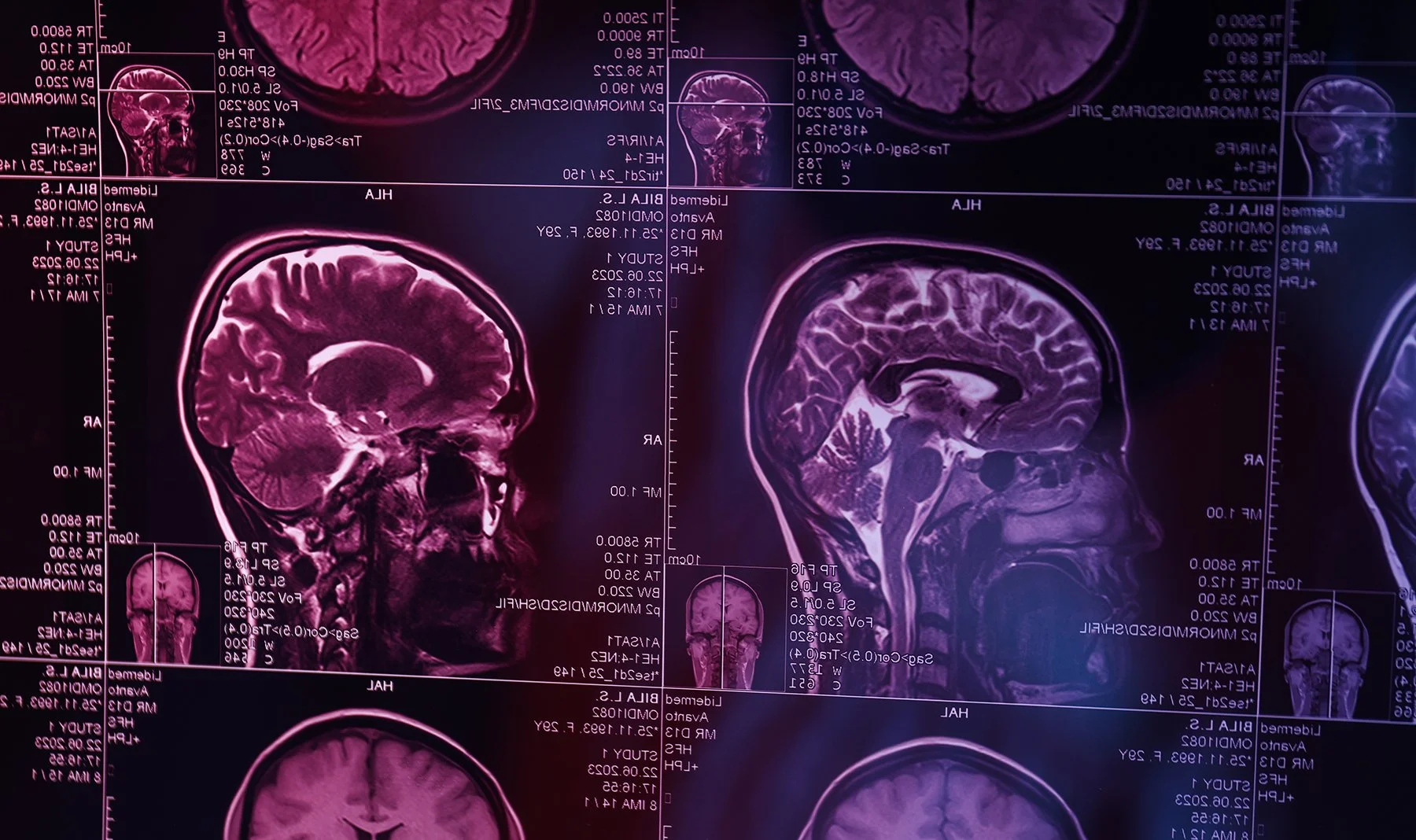
MRI in suspected trigeminal neuralgia to look for possible causes like vascular compression and to help rule out other causes such as multiple sclerosis or a tumor (your clinician decides based on your case). [4]
Condition-specific evaluation when symptoms point toward other diagnoses (for example, giant cell arteritis needs urgent evaluation due to the risk of vision loss). [13]
Step 7: When facial pain is likely nerve-related
If your pain is:
shock-like,
one-sided,
triggered by light touch/chewing/talking,
and recurring in bursts,
that’s a pattern that should raise suspicion for trigeminal neuralgia, and it’s worth getting evaluated by a specialist who routinely treats cranial nerve disorders. [2][3]
Why a specialist evaluation can save time
Facial pain is a symptom with many possible causes, including headaches, sinus infections, dental issues, nerve disorders, and other medical conditions. The goal is not just “pain relief,” but getting the correct label so treatment matches the cause. [1]
Facial pain evaluation in NYC
If you’re dealing with recurring facial pain and you suspect trigeminal neuralgia or another nerve-related cause, consider a specialist evaluation.
Dr. Ramesh P. Babu is a board-certified neurosurgeon and Director of Neurosurgery at BronxCare Health System, with a clinical focus that includes trigeminal neuralgia and facial pain. [15][16] His practice outlines a diagnostic approach that includes a detailed neurologic evaluation and the use of advanced MRI imaging when appropriate to look for nerve compression or other underlying causes. [17]
References & Resources
Cleveland Clinic. Facial Pain: Types, Causes & Treatment.
https://my.clevelandclinic.org/health/symptoms/facial-pain Cleveland ClinicNational Institute of Dental and Craniofacial Research (NIDCR). Trigeminal Neuralgia.
https://www.nidcr.nih.gov/health-info/trigeminal-neuralgia NIDCRMayo Clinic. Trigeminal neuralgia: Symptoms and causes.
https://www.mayoclinic.org/diseases-conditions/trigeminal-neuralgia/symptoms-causes/syc-20353344 Mayo ClinicMayo Clinic. Trigeminal neuralgia: Diagnosis and treatment (includes MRI use).
https://www.mayoclinic.org/diseases-conditions/trigeminal-neuralgia/diagnosis-treatment/drc-20353347 Mayo ClinicMayo Clinic. TMJ disorders: Symptoms and causes.
https://www.mayoclinic.org/diseases-conditions/tmj/symptoms-causes/syc-20350941 Mayo ClinicMayo Clinic. Acute sinusitis: Symptoms and causes.
https://www.mayoclinic.org/diseases-conditions/acute-sinusitis/symptoms-causes/syc-20351671 Mayo ClinicAmerican Migraine Foundation. Migraine Signs & Symptoms.
https://americanmigrainefoundation.org/migraine-signs-symptoms/ American Migraine FoundationMayo Clinic. Cluster headache: Symptoms and causes.
https://www.mayoclinic.org/diseases-conditions/cluster-headache/symptoms-causes/syc-20352080 Mayo ClinicCDC. Clinical Features of Shingles (Herpes Zoster) (includes PHN definition and facial involvement).
https://www.cdc.gov/shingles/hcp/clinical-signs/index.html CDCInternational Headache Society. ICHD-3: Persistent idiopathic facial pain (PIFP).
https://ichd-3.org/13-painful-cranial-neuropathies-and-other-facial-pains/13-12-central-neuropathic-pain/ ICHD-3Cleveland Clinic. Tooth Abscess: Symptoms, Causes & Treatments.
https://my.clevelandclinic.org/health/diseases/10943-abscessed-tooth Cleveland ClinicAmerican Stroke Association. F.A.S.T. Materials (Stroke warning signs).
https://www.stroke.org/en/help-and-support/resource-library/fast-materials www.stroke.orgMayo Clinic. Giant cell arteritis: Symptoms and causes.
https://www.mayoclinic.org/diseases-conditions/giant-cell-arteritis/symptoms-causes/syc-20372758 Mayo ClinicMedlinePlus. Orbital cellulitis (medical emergency guidance).
https://medlineplus.gov/ency/article/001012.htm MedlinePlusBronxCare Health System. Ramesh Babu, M.D. (Director, Neurosurgery).
https://www.bronxcare.org/physicians/find-a-physician/detail/ramesh-babu/ bronxcare.orgNYC Brain Surgery. Dr. Ramesh Babu, NYC Neurosurgeon.
https://nycbrainsurgery.org/dr-ramesh-babu-nyc-neurosurgeon nycbrainsurgery.orgNYC Brain Surgery. Facial Pain Specialist NYC (diagnostic approach including MRI use).
https://nycbrainsurgery.org/facial-pain nycbrainsurgery.org