Trigeminal Neuralgia: Symptoms, Diagnosis, and Treatment in NYC
Trusted care with Dr. Ramesh P. Babu, M.D., Board-Certified Neurosurgeon
Trigeminal neuralgia causes sudden, electric shock-like facial pain that can stop your day. If you are feeling sharp facial pain triggered by light touch, chewing, or even a breeze, you may have a highly treatable condition. Dr. Ramesh Babu is a New York City neurosurgeon with decades of experience helping patients find lasting relief.
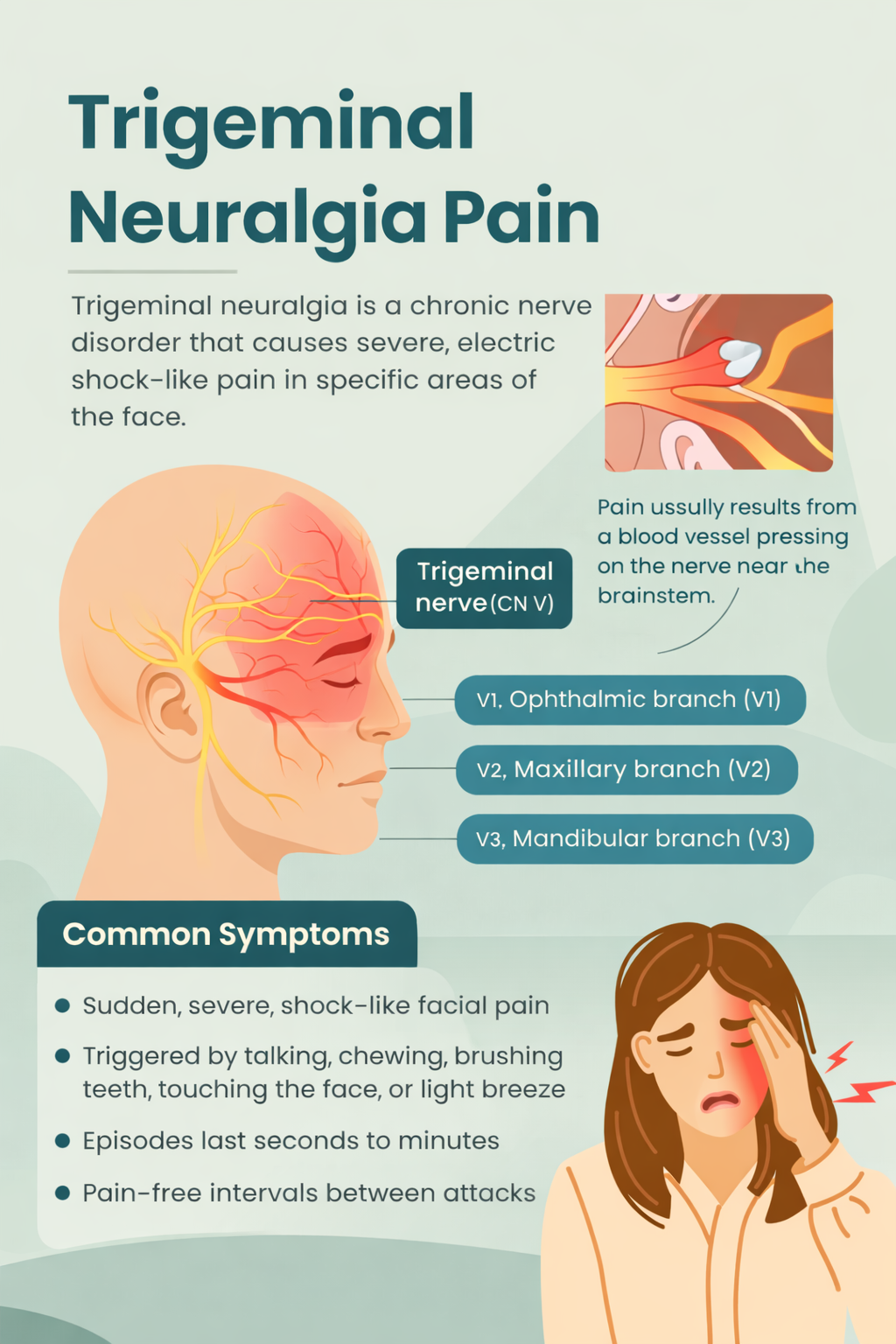
What is trigeminal neuralgia?
Trigeminal neuralgia (TN) is a nerve pain disorder that affects the trigeminal nerve, which carries sensation from your face to your brain. In classic TN, a small blood vessel presses on the nerve near the brainstem. This “neurovascular compression” irritates the nerve and causes painful misfiring.
Key facts
Pain is usually one-sided in the cheek, jaw, lip, teeth, or around the eye
Attacks last seconds to minutes and may cluster in bursts
Triggers include light touch, brushing teeth, talking, eating, or wind
Symptoms
Sudden, stabbing, shock-like facial pain
Short attacks with pain-free intervals
Trigger points on the face that set off pain with gentle contact
Heightened sensitivity after attacks
Anxiety or avoidance of eating, speaking, or hygiene due to fear of pain
Call us if you notice constant burning facial pain, facial numbness, or pain on both sides. These can occur in other facial pain disorders and need a careful evaluation.
Who gets TN?
TN is more common after age 50 but can occur at any age. It affects women slightly more often than men. Rarely, TN is associated with multiple sclerosis or a structural problem. Most patients have classic TN due to a blood vessel touching the nerve.
How TN is diagnosed
Diagnosis is clinical, based on your history and exam. Dr. Babu will confirm the pattern of brief, triggerable, one-sided pain and rule out dental or sinus causes.
Imaging
MRI of the brain with trigeminal nerve protocol to look for vascular compression and rule out other causes
Typical protocol includes high-resolution 3D T2 (CISS/FIESTA), time-of-flight MRA, and contrast-enhanced T1 when indicated.Imaging also helps guide treatment selection.
First-line treatment
Most patients start with medication that calms the nerve.
Carbamazepine or oxcarbazepine are the usual first choices
Dr. Babu monitors dosing, side effects, and bloodwork as needed
Some patients benefit from add-on medicines such as baclofen, lamotrigine, or gabapentin
Genetic screening for HLA-B*15:02 is recommended in at-risk ancestries before starting carbamazepine due to rare but serious skin reactions
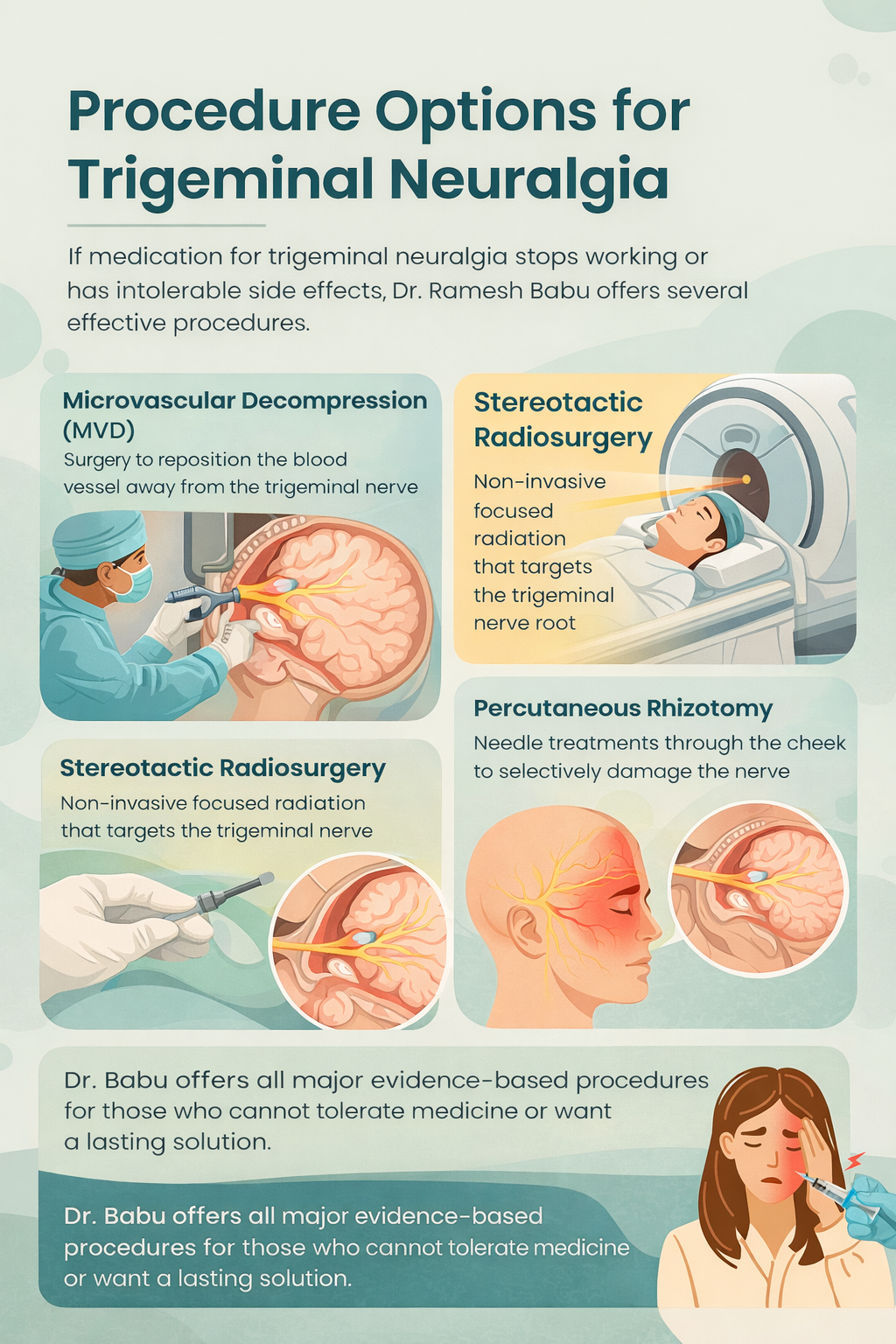
If medicines stop working, cause side effects, or do not control attacks, procedural options offer durable relief.
Procedure options
Dr. Babu offers the full range of evidence-based treatments and will help you choose based on your health, imaging, and goals.
Microvascular decompression (MVD)
Microsurgery that moves the offending blood vessel away from the nerve and cushions it
Highest chance of long-term, medication-free relief in classic TN
Requires general anesthesia and a short hospital stay
Stereotactic radiosurgery (Gamma Knife or similar)
Outpatient, noninvasive focused radiation to the trigeminal root
Lower upfront risk, often preferred for older patients or those avoiding open surgery
Pain relief may be gradual over weeks
Percutaneous rhizotomy procedures
Needle-based treatments done through the cheek to partially disrupt pain fibers
Radiofrequency ablation
Balloon compression
Glycerol rhizolysis
Fast recovery and repeatable if pain returns
Botulinum toxin injections
Targeted injections at facial trigger zones can reduce attacks for 3 to 6 months
Useful when medicines are not tolerated or as a bridge to a longer-term option
What outcome can I expect?
Many patients regain normal daily life. The best outcomes occur when treatment is matched to the cause and severity.
Classic TN with clear vascular compression often responds best to MVD
Radiosurgery and percutaneous options are effective alternatives with different risk and durability profiles
If pain recurs, you still have options
Dr. Babu will review benefits, risks, and recovery details for each approach so you can decide with confidence.
When to see a neurosurgeon
You have classic triggerable facial pain that medicines do not control
You cannot tolerate medication side effects
Your pain pattern is changing, or you notice numbness or weakness
You want to understand the full range of definitive options
Early consultation prevents months of uncontrolled pain and helps protect nutrition, sleep, and mental health.
Why patients choose Dr. Ramesh Babu in NYC:
Board-certified neurosurgeon with deep expertise in cranial nerve disorders
Comprehensive evaluation with high-resolution MRI protocols
All major TN procedures available, matched to your needs
Clear, patient-first counseling and shared decision-making
Care across New York City, including Brooklyn and the Bronx
What to expect at your visit:
Focused history and neurological exam
MRI review or new imaging order if needed
Stepwise plan: medication optimization, interventional options, or surgery
Education on triggers, oral care, and pain safety
Direct contact for follow-up and flare support
FAQs
Is trigeminal neuralgia dangerous?
TN is very painful but not life-threatening. The goal is fast, safe control of attacks and prevention of disability.
Will I need surgery?
Not always. Many patients do well on medication. Surgery or radiosurgery is considered when pain persists or side effects limit dosing.
How do I know if I have classic TN or atypical facial pain?
Classic TN has brief, shock-like attacks with triggers and pain-free intervals. Constant burning pain suggests atypical facial pain or a mixed picture. A specialist exam helps clarify this.
Can dental problems cause similar pain?
Yes. Dental disease and TMJ disorders can mimic TN. A careful exam and sometimes dental evaluation are part of the workup.
What are the risks of MVD?
MVD has the highest chance of long-term relief in classic TN. Risks include infection, bleeding, hearing changes, facial numbness, spinal fluid leak, or stroke, which are uncommon in experienced hands.
How soon does radiosurgery work?
Relief is often gradual over weeks to a few months. Some patients need medication during the transition.
Do injections help?
Botulinum toxin injections at trigger sites can reduce attacks for several months. They can be repeated and combined with other treatments.
Will TN come back?
It can. If pain recurs, repeat imaging and a tailored plan usually restore control.
Can TN affect both sides?
It is usually one-sided. Bilateral pain is uncommon and needs careful evaluation for other causes.
Is this the same as cluster headache or migraine?
No. Those are different headache disorders. The exam and history help distinguish them.