What Can Be Mistaken for Trigeminal Neuralgia? Symptoms, Look-Alikes, and What to Do
Trigeminal neuralgia (TN) causes sudden, electric-shock facial pain that can be terrifying to experience and easy to misdiagnose. This guide explains what TN feels like, common conditions that mimic it, how doctors tell them apart, and what you should do next—with references to authoritative medical sources.
Quick definition: what trigeminal neuralgia feels like
Pain quality: electric-shock, stabbing, or shooting.
Duration: attacks last fractions of a second up to 2 minutes and may repeat in clusters through the day.
Side & location: usually one side of the face, most often cheek or jaw (V2/V3).
Triggers: light, innocuous touch (breeze, brushing teeth), speaking, chewing.
Between attacks: many are pain-free; some have a dull background ache.
Work-up: high-resolution MRI is recommended for all suspected cases to rule out secondary causes and look for a compressing blood vessel.
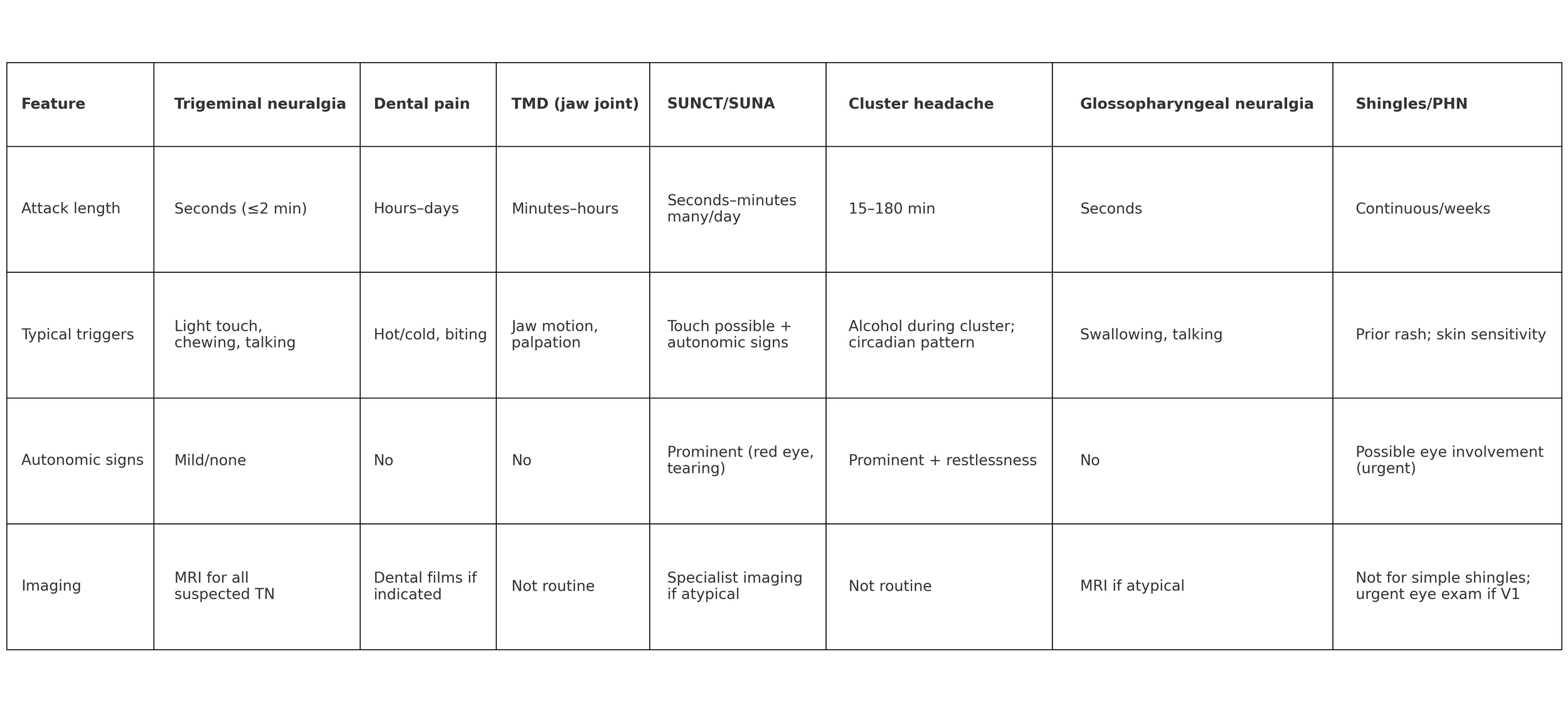
Conditions commonly mistaken for TN—and the key differences
Pay attention to attack length, triggers, autonomic signs (tearing/red eye/runny nose), continuous vs brief pain, and exam/imaging.
1) Dental pain (pulpitis, cracked tooth, abscess)
Typical: throbbing, continuous tooth-localized pain; worse with hot/cold or biting; dental exam often finds a culprit tooth and treatment helps.
Clues against TN: lacks seconds-long shocks and light-touch triggers; not strictly along trigeminal “divisions.”
Why it matters: misdiagnosis can lead to unnecessary root canals/extractions that don’t help TN pain. Royal College of Surgeons
2) Temporomandibular disorders (TMD)
Typical: dull ache at jaw joint/temples; clicking, locking, or limited opening; pain provoked by jaw movement or muscle palpation; episodes last minutes–hours.
Clues against TN: not shock-like; usually no light-touch trigger zones; can be bilateral.
Evidence base: DC/TMD diagnostic criteria. ubwp.buffalo.edu
3) Sinusitis
Typical: nasal congestion + colored discharge, reduced smell, facial pressure worse with bending forward; lasts days–weeks.
Clues against TN: pressure-like, prolonged pain; no electric shocks or light-touch triggers. nhs.uk
4) Trigeminal autonomic cephalalgias (TACs): SUNCT/SUNA and cluster headache
SUNCT/SUNA: seconds–minutes, many times per day + prominent autonomic signs (red eye, tearing, runny nose).
Cluster headache: 15–180-minute attacks around the eye/temple with tearing, nasal congestion, droopy eyelid and restlessness; occur in “clusters” for weeks.
Clues against TN: TACs show prominent eye/nose symptoms; cluster lasts much longer than TN. ICHD
5) Migraine that presents as facial pain (orofacial migraine)
Typical: hours-long throbbing or pressure pain that may sit in the upper/lower jaw, teeth, or cheek, often with nausea and light/sound sensitivity—not light-touch triggers.
Clues against TN: attacks last much longer; sensory sensitivity to light/sound rather than to gentle touch. MDPI
6) Glossopharyngeal neuralgia
Typical: electric pain in throat/tonsil, back of tongue, ear, triggered by swallowing, speaking, coughing.
Clues against TN: different location and swallowing-related triggers. International Headache Society
7) Shingles & post-herpetic neuralgia (especially herpes zoster ophthalmicus, V1)
Typical: burning or aching pain with skin sensitivity, following (or occasionally preceding) a unilateral blistering rash on the forehead/eyelid; eye involvement can threaten vision.
Clues against TN: continuous neuropathic pain and a rash history; urgent eye care if eyelid/eye involved. CDC
8) Painful post-traumatic trigeminal neuropathy (after dental work, facial trauma, nerve block)
Typical: persistent burning/aching pain with numbness or altered sensation in a trigeminal territory after a procedure or injury.
Clues against TN: sensory deficit and ongoing pain tied to a clear preceding event. BioMed Central
9) “Secondary TN” from multiple sclerosis or skull base/cerebellopontine angle tumors
Typical: TN-like attacks with additional neurologic signs (facial numbness, hearing loss, imbalance), bilateral TN (more common with MS), or younger onset.
Key point: MRI is recommended for all suspected TN to exclude these causes and to evaluate for neurovascular compression. uems-neuroboard.org
How clinicians confirm TN (what to expect)
Detailed history & exam: mapping pain to V1/V2/V3, checking trigger zones, and screening for sensory loss or other neurologic signs (ICHD-3 overview).
MRI with high-resolution trigeminal sequences (e.g., CISS/FIESTA) to rule out tumors or MS and to look for neurovascular compression in “classical” TN (Practical Neurology review).
First-line medication trial: carbamazepine or oxcarbazepine; early benefit supports the diagnosis. Opioids are not recommended (EAN guideline).
What to do if you have these symptoms
Avoid irreversible dental work (extractions/root canals) unless there is clear dental disease and TN has been considered—misdiagnosis is common (RCS guideline; cohort study on unnecessary dental procedures in TN: Surgical Neurology International).
See a specialist experienced in facial pain (neurologist, neurosurgeon, or orofacial pain specialist) and ask about MRI as part of the work-up (EAN guideline). UEMS Neuroboard
Track your attacks for a few days: duration (seconds vs minutes/hours), triggers (light touch vs chewing vs hot/cold), autonomic signs (tearing, red eye, runny nose), location (eye/cheek/jaw), and any rash or numbness. This helps your clinician distinguish TN from mimics (ICHD-3 framework).
Seek urgent care now if you have
Rash on forehead/eyelid or new eye pain/vision changes → possible zoster ophthalmicus, which needs same-day antivirals and urgent eye evaluation (CDC; AAO).
New neurologic signs, bilateral facial shocks, or you’re younger with new TN symptoms → prompt MRI and specialist review (EAN guideline).
Care in New York City
If you’re experiencing shock-like facial pain or a confusing mix of symptoms, Dr. Ramesh P. Babu, M.D. evaluates trigeminal neuralgia, skull base tumors, and other causes of facial pain. We coordinate imaging, confirm the diagnosis, and discuss medication and procedural options to get you relief.
References
Headache Classification Committee of the International Headache Society. ICHD-3:
Trigeminal neuralgia: https://ichd-3.org/13-painful-cranial-neuropathies-and-other-facial-pains/13-1-trigeminal-neuralgia/13-1-1-classical-trigeminal-neuralgia/. ICHD-3
SUNCT/SUNA: https://ichd-3.org/3-trigeminal-autonomic-cephalalgias/3-3-short-lasting-unilateral-neuralgiform-headache-attacks/3-3-1-short-lasting-unilateral-neuralgiform-headache-attacks-with-conjunctival-injection-and-tearing-sunct/. ICHD-3
Cluster headache: https://ichd-3.org/3-trigeminal-autonomic-cephalalgias/3-1-cluster-headache/ and https://ichd-3.org/3-trigeminal-autonomic-cephalalgias/3-1-cluster-headache/3-1-1-episodic-cluster-headache/. ICHD-3+1
Glossopharyngeal neuralgia: https://ichd-3.org/13-painful-cranial-neuropathies-and-other-facial-pains/13-2-glossopharyngeal-neuralgia/13-2-1-glossopharyngeal-neuralgia/. ICHD-3
Painful post-traumatic trigeminal neuropathy: https://ichd-3.org/13-painful-cranial-neuropathies-and-other-facial-pains/13-1-trigeminal-neuralgia/13-1-2-painful-trigeminal-neuropathy/13-1-2-3-painful-post-traumatic-trigeminal-neuropathy/. ICHD-3
European Academy of Neurology (2019) Guideline on Trigeminal Neuralgia: https://www.uems-neuroboard.org/web/images/docs/exam/2021/Guideline-Papers/EAN-guideline-trigeminal-neuralgia-Bendtsen2019.pdf. UEMS Neuroboard
Royal College of Surgeons (UK) 2021 — Trigeminal Neuralgia Guideline: https://www.rcseng.ac.uk/-/media/files/rcs/fds/guidelines/trigemina-neuralgia-guidelines_2021_v4.pdf. Royal College of Surgeons
Maarbjerg S, et al. Trigeminal neuralgia: a practical guide. Practical Neurology 2021: https://pn.bmj.com/content/21/5/392. BMJ Paediatrics Open
CDC — Clinical overview of shingles (herpes zoster): https://www.cdc.gov/shingles/hcp/clinical-overview/index.html. CDC
American Academy of Ophthalmology — Herpes zoster ophthalmicus pearls: https://www.aao.org/eyenet/article/herpes-zoster-ophthalmicus-pearls. AAO
NHS — Sinusitis (sinus infection): https://www.nhs.uk/conditions/sinusitis-sinus-infection/. nhs.uk
DC/TMD diagnostic criteria — Schiffman et al., J Oral & Facial Pain and Headache: https://files.jofph.com/files/article/20231214-383/pdf/ofph_28_1_Schiffman_02.pdf. Jofph Files
Orofacial migraine — MDPI narrative review: https://www.mdpi.com/1660-4601/20/20/6946; facial-pain cohort (Neurology PDF): https://orofacialpain.org.uk/wp-content/uploads/2021/11/Link-3-Facial-presentations-TACs-migraine.pdf. MDPI+1
Post-traumatic trigeminal neuropathic pain — Biomedicines review (2024): https://www.mdpi.com/2227-9059/12/9/2058. MDPI
Unnecessary dental procedures in TN — Surgical Neurology International study: https://surgicalneurologyint.com/surgicalint-articles/please-spare-my-teeth-dental-procedures-and-trigeminal-neuralgia/. Surgical Neurology International